Welcome to Part 2 of My Eczema Baby series. In Part 1 of My Eczema Baby Series, I offered 9 ways to immediately alleviate your baby’s eczema symptoms. That post covered the tried and true methods and products that really helped make a difference in Nugget’s day-to-day eczema management.
In this post, I’m sharing our 6+ month journey to uncover what caused Nugget’s eczema and what we did to manage her flare-ups. While managing symptoms offered temporary relief, we didn’t see a significant difference until we combined diet modification with a strict skincare regimen. I tried to cover all the things in this post, such as:
- how we identified her eczema
- diet elimination and other steps we took to manage her flare-ups
- what to expect from allergy testing
- questions I had for the allergist
- what we’ve learned from experience and through extensive research on our eczema journey
- links to further research you may want to check out
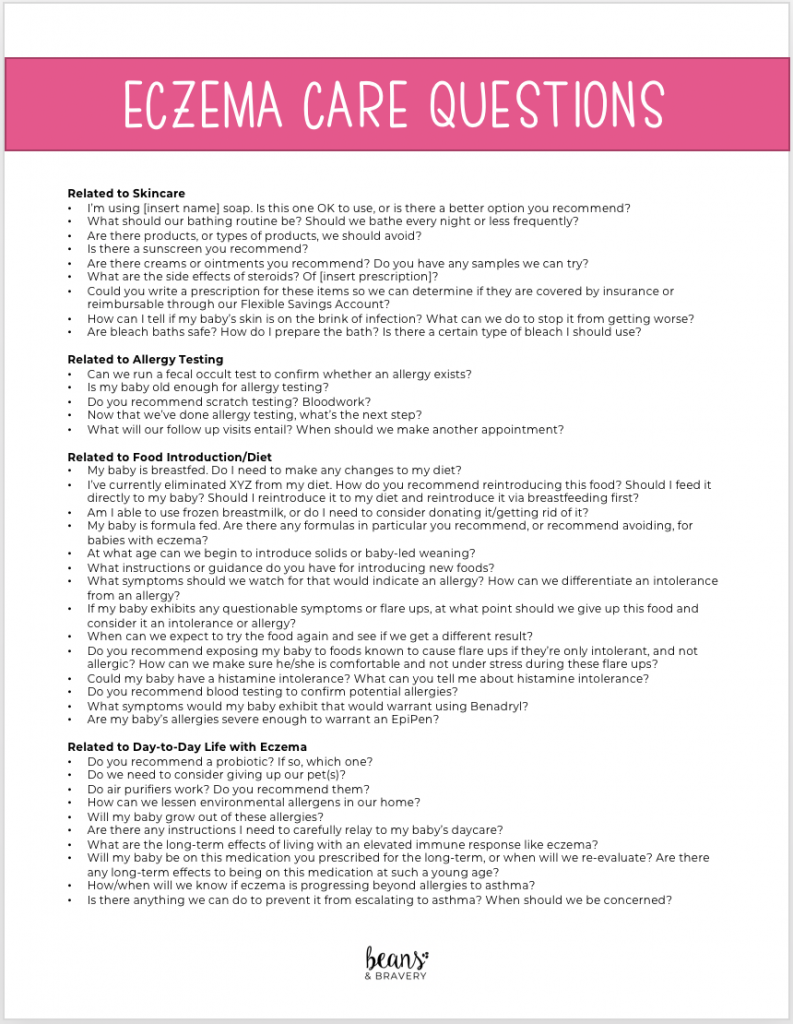
I’ve asked SO MANY questions along the way, that I’ve also included for you my handy master list of questions for your next appointment with a pediatrician or allergist. But in the meantime, feel free to drop me a question in the comments section below and I’ll respond with our experience.
This post is not meant to serve as medical advice. Please consult your child’s pediatrician or allergist for the best path forward for your baby.
Also, while this post may contain affiliate links for which I may receive a small commission, I only recommend products that I’ve tried and loved.
What’s causing my baby’s eczema?
When you have a baby with eczema, you’re often thinking simply, “how do I make it go away?” I must have Googled this question a thousand times. I was only left with more questions, frustrated by answers such as “genetics,” and conflicting information about whether diet was a factor.
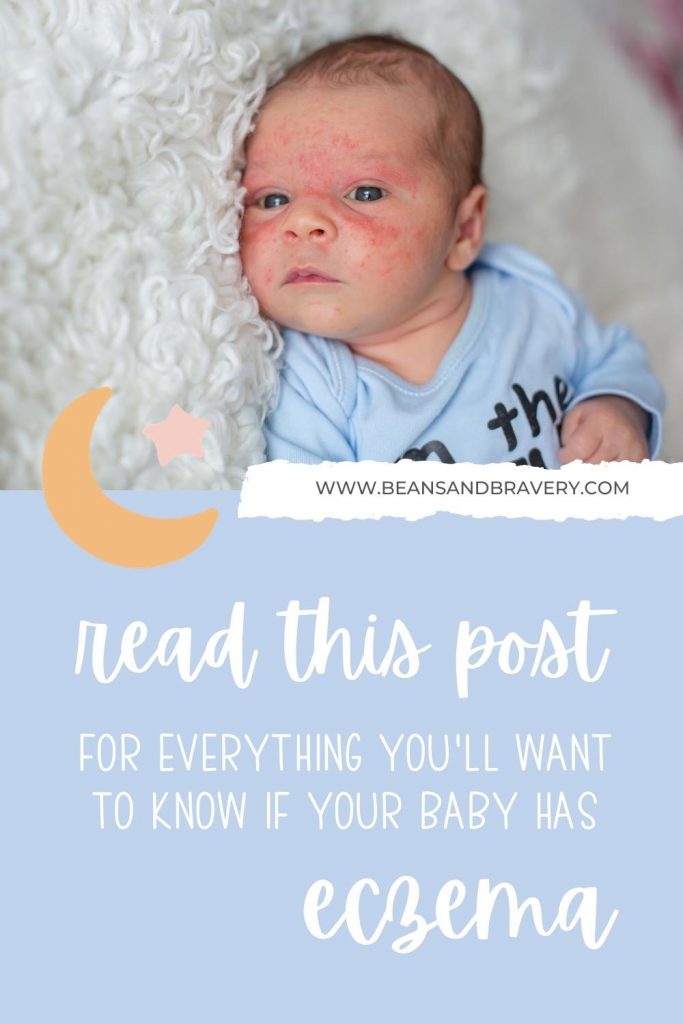
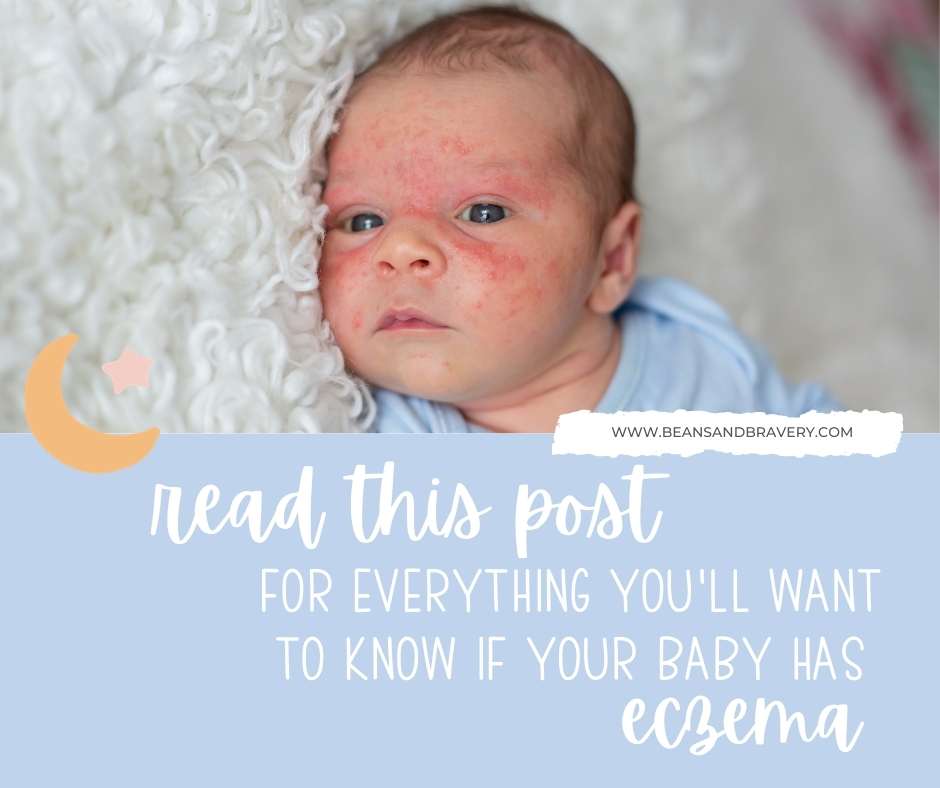
Children with eczema, also known as atopic dermatitis (AD), will develop patches of dry, itchy, scaly skin caused by allergic inflammation. Symptoms range from minor itchiness to extreme discomfort. These symptoms can be so severe that they disrupt sleep. Constant scratching can exacerbate already sensitive skin, and lead to recurrent infections in scratched, broken skin. We experienced all of these things.
Nugget’s skin was scaly, red, itchy and she was, at times, inconsolable. One evening while changing a poopy diaper, I noticed blood streaks and freaked out. What was a concern I was going to bring up at her next well visit (her skin) became an immediate call to the pediatrician. Blood in poop, I knew, was not normal.
The nurse on call suggested bringing the diaper in for a fecal occult test. While we waited for the results, our pediatrician tried to reassure us that most babies do not have dairy allergies. This could be a fluke. But it came back positive, which indicated bleeding in her digestive tract, or allergic colitis. She was allergic to something I was eating, and it was causing her digestive tract such upset that she was experiencing a bloody gut.
We had the first piece of information we needed: she was allergic to dairy or soy.
Can I breastfeed a baby with eczema?
When visible blood is found in a baby’s poop, it is often because of cow-milk/soy protein-induced allergic colitis. This can be the case for an exclusively breast-fed (EBF) baby, or a baby fed formula, which is usually made from milk proteins.
We discussed options with our pediatrician. Our little one was EBF and I wished to continue breastfeeding. It was the recommended option since she was just 8 weeks old. Most formulas are made from dairy or soy, which isn’t recommended for babies under six months. The alternate formulas were known to taste awful and were very expensive.
So, I needed to cut out all dairy products. No more Hormel protein packs I lived on for quick snacks. Or daily ice cream desserts. No more butter on my toast. Or cream cheese on my bagels. No sour cream on my nachos. Or quick pizza Friday dinners when I was exhausted and too tired to cook. And no more chocolate.
It also meant the freezer stash of breast milk I had saved up to this point was unusable for the foreseeable future. I had to start over, unsure of whether we’d ever be able to touch the supply we had overtaking our freezer. While 80% of children will grow out of a dairy allergy by age 3, breast milk is only recommended to be frozen up to a year. Waiting for results would be tedious. It could take up to six weeks for traces of dairy to leave my system, and then hers. There were no cheat days.
I’d have to wait six weeks to start building a new stash free from dairy. And all of this was happening as I was getting ready to go back to work.
Little did we know, the positive test result would begin a 6-month journey to try to identify her triggers.
We began our dairy elimination journey as a first step. Soy elimination would follow if there was no improvement.
Will dairy elimination prevent infant eczema?
A few days dairy free, and alongside topical treatment of Mupirocin antibiotic ointment, we saw drastic improvement. Her face had gone from red, angry and crusty to smooth, pale baby skin. The results made the sacrifice worth it. She was happier and so was I (and so was dad)!
Related Post: Suspect your eczema baby has a milk allergy? You’ll want to read this post.
Then, as quickly as she got better, she got worse.
Her skin returned to its pre-dairy elimination state. Days passed by. Then weeks. I was strictly adhering to a dairy-free diet, logging my meals and snacks. I was unhealthily dropping weight. My breast milk supply tanked. And I was frustrated by the lack of results, while needing to adapt to a new lifestyle free from my favorite foods.
“Give it some time,” her pediatrician said. We waited. We saw no improvement.
I reached back out at the six week mark, when she was just over three months old. Her pediatrician was concerned that we hadn’t yet seen meaningful results. She suggested we were likely looking at a multiple allergy situation. My heart sank. It was time to eliminate soy, too.
Results fluctuated, but nothing kept her skin clear for long. Soy was the most difficult to avoid of all the allergens I eliminated on this journey. Soy is in nearly everything prepared or packaged. When I gave up soy, I needed to take on meal prepping and planning. My husband had gone back to work. My maternity leave was ending. I was trying to take care of a newborn, prep all of her needs for daycare, and prep enough food to sustain my milk supply. It was extremely difficult, and frustrating that we still didn’t have answers.
Should a baby with eczema get allergy testing?
Allergy testing was out of the question until Nugget was closer to six months old. She was simply too young and it wasn’t recommended. So diet elimination was our best bet to identify what was causing her distress.
When eliminating dairy on its own didn’t work, it was onto the next food group, one-by-one, until I eliminated them all. If eliminating food groups one at a time wouldn’t work or provide answers, I was going to eliminate them all and add them back in one-by-one, until we identified which triggers caused her flare ups.
At one point, I had eliminated all major allergens and anything else I could tie back to a flare-up from my persistent food journaling. This included dairy, wheat, eggs, soy, peanuts, citrus, tomatoes, and more.
Download Now: Food Journal Template
We were eating chicken, potatoes, and [insert vegetable here] night after night. We couldn’t eat out. Or order in. No matter how careful I was to ask questions about ingredients, it was never careful enough. Allergies aren’t taken nearly as seriously as they should be by food establishments. So our date nights disappeared and so did our social outings with friends. You don’t realize how many social gatherings center around food until you’re faced with dietary restrictions. On the rare occasion we did go out, I would eat beforehand and keep carrot sticks in my bag for emergencies.
Month after month we would check in with our pediatrician. Her skin was always red and angry, but she was still a happy baby. Sometimes she needed antibiotic ointment as her skin teetered on infection. Other times, it calmed down using over-the-counter creams and hydrocortisone ointment.
When is a baby old enough for an allergist appointment?
As she was nearing turning five months old, it was time to pursue a pediatric allergist appointment. A call to DuPont and CHOP left me feeling helpless as the soonest we could get in was two months away. She was finally old enough to do allergy testing and we had to wait even longer.
Thankfully, a local private practice could fit us in the following week. Two-and-a-half hours of testing and discussions later, we had results from a skin prick test: she was allergic to dairy, eggs, and our cat–the one constant factor she was exposed to that I had been unable to eliminate.
What to expect at an allergist appointment
Our allergist started by taking a thorough history of my dietary eliminations. I had gotten a head start and had been eliminating various foods for about three months at this point. Arriving with a food journal and log of her symptoms provided a helpful starting point for our discussion and a direction for Nugget’s testing. (If you’d like to start your own, you can download my template here.)
He asked questions about what I had eliminated, what type of symptoms she had, and specific questions about her changes in skin and breathing when she had reactions. The more detailed you can be, the better. At our pediatrician’s recommendation, because we were not seeing results, we had not yet added any eliminated foods back in. I was looking to get advice from the allergist about how to safely do so.
While Nugget could have been allergic to more than just dairy, eggs and our cat, we tested only 14 allergens because her body was so red and flared up. We were limited to prick only the clear patch of skin on her back. He chose to test for the most common allergens (dairy, soy, egg, wheat, peanuts, coconut, dogs, cats) and also chose other foods based on what I was currently eating. This is because her skin was not getting better and my diet was already so limited. The hypothesis was that she was either allergic to something I was eating in my already limited diet–or it was another factor such as something environmental (the cat, dog, dust, pollen, etc.).
Is the allergist invasive or painful?
The prick test was relatively quick. He cleaned her back, used a pen to mark where he would prick, and then pricked the spots with each potential allergen. (Speaking from experience, it feels like a scratch from a hair brush.) We waited 15-20 minutes for reactions. He then measured each spot that flared up and assigned it a number that essentially correlated to how allergic she likely was to the allergen. After he was finished, he cleaned off her back and gave her an antihistamine to calm her itchy spots.
Armed with new information about her allergens, we then had a discussion about what to do next. We were prescribed a mild topical steroid, and an after-bath routine of hydrocortisone, CeraVe cream (or Vanicream as an alternative), and Vaseline. And, he recommended adding regular bleach baths to our routine.

I was very concerned about the steroid use having read that babies’ skin can become dependent upon it, but our allergist put things into perspective: Uncontrolled flare-ups and regular antibiotic use was far worse for a baby than as-needed, tapered steroid use to control flare-ups. Because she also would be exposed to our cat, she was prescribed daily doses of Children’s Zyrtec. Adding Zyrtec to her routine was the game-changer for eliminating flare-ups that resulted from constant exposure to the cat.
The allergist was wonderful and thorough in answering all of my questions. We swore she reacted on the days I ate peanut butter–but she didn’t react at all to the test. Could she still be allergic to them? Did my diet still matter? How could we safely reintroduce foods I had been avoiding up to this point? Could we still introduce foods to her starting at six months? Do we need to give up our cat? Will she grow out of these allergies? Do air purifiers work? What do we do next? I had so many questions and he answered them all.
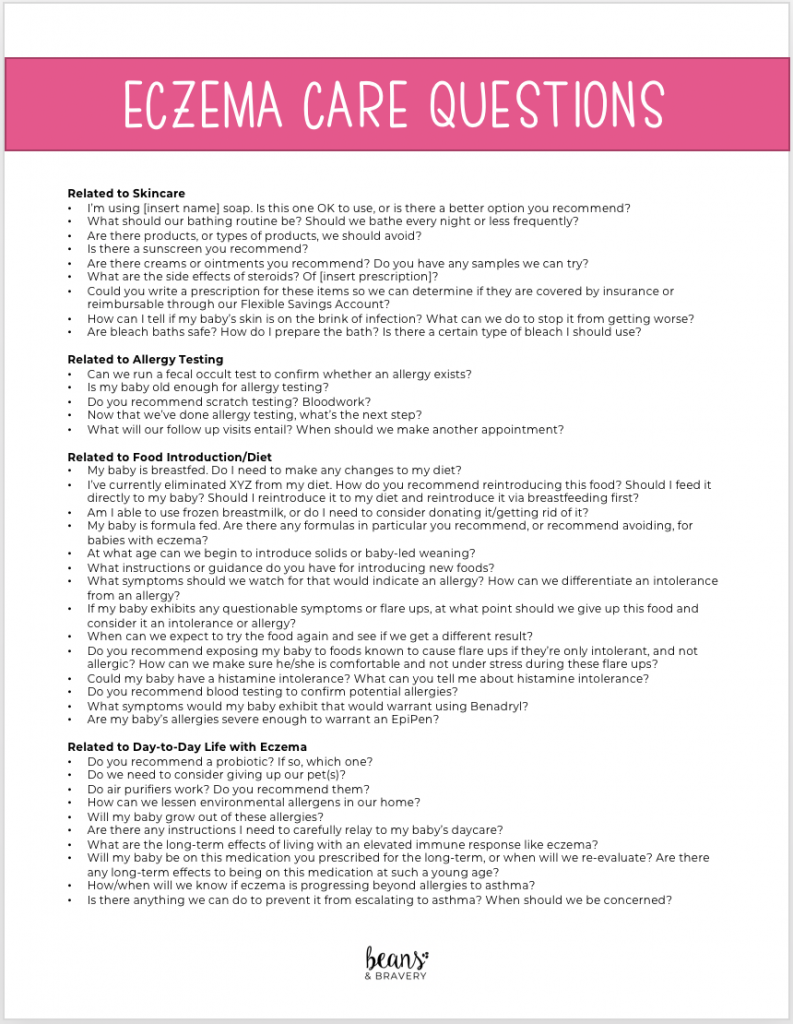
Download my master list of questions to take to your own appointment here.
What we’ve learned from studies, allergist appointments, and experience
You’ll soon find out, if you haven’t already, that there is conflicting information on the internet about what causes eczema. And like many skin regimens, what works for one person may or may not work for another. I have been where you are, mama! Frustrated, overwhelmed, and desperate for answers. Below I’ve summarized what I’ve learned along our journey to hopefully help you on yours.
- Allergy testing may or may not give you answers. Learning about the allergy to our cat put everything into perspective. It wasn’t cut-and-dry dietary allergies like I had suspected. An environmental allergy was not something we necessarily would have predicted, but it was the consistent factor that kept Nugget from clear skin.
Allergy testing can be done via scratch testing or blood testing. The most non-invasive way for babies is scratch testing, and it usually won’t be performed under six months. Scratch testing, or skin prick testing, is limited in that it may not reveal what causes eczema flare-ups, only what is an actual allergy. Also, skin must be clear enough to do the testing. This can be a challenge for babies suffering from full-body flare ups. Allergies are identified when they surpass a given number in terms of severity. If the scratch test spot reddens to a certain measurement, it’s considered an allergy.
Blood testing is usually the more reliable method for identifying antibody response to allergens. But is usually not performed on infants because their veins are difficult to access and more than one vial is often required. Some allergists may recommend confirmatory blood testing, or recommend it under circumstances when scratch testing is not right for your baby. In this case, request a pediatric phlebotomist who is used to drawing blood from infants.
We’ll never know which was the chicken and which was the egg. Was her eczema caused by her allergy to the cat? Or was her dairy allergy the main cause of her flare-ups, and her allergy to the cat was the result of her exposure while her skin was damaged? We suspect the dairy allergy came first, since most children develop a tolerance to pets through exposure. Which brings me to #2. - Children with eczema are at risk of developing allergies through skin exposure. According to the National Eczema Association “immune cells in the skin prompt a variety of other cells to form, which cause allergy.” It is still unknown whether food allergies make eczema worse. Or if injured skin makes way for intolerances to food. But by keeping a strict skin regimen, you can mitigate the likelihood of developing allergies through skin exposure. This is why, regardless of whether you see a pediatric allergist or dermatologist first, both are likely to recommend starting and adhering to a strict skincare regimen.
We experienced this not only with exposure to the cat’s dander, but also with oatmeal once we began exposing Nugget to foods. After two weeks of eating oatmeal nearly three times a day without issue, she suddenly refused to eat it and would flare up horribly when she nursed (it was all I ate for breakfast). This is when I learned allergies to foods can develop if they’re introduced to damaged skin. We had to eliminate oatmeal from both of our diets until she was nearly a year old and her reaction to it had subsided. - The skin mirrors gut health. If your gut is unhealthy, your skin will be, too. Which is why dietary restrictions can be necessary for managing eczema. However, some flare-ups are to be expected for babies when introducing new foods as their GI tract develops and gets used to being exposed to new foods. But it’s the severity that matters. When babies are in the sweet spot of 8-12 months, it’s important to expose them to a variety of foods so that they don’t become allergic, which can happen if foods are avoided completely. It’s a very careful balance which is why consulting your pediatrician and allergist for guidance for your baby’s unique situation is important.
- Probiotics are a good thing. The allergist also recommended starting Nugget on a probiotic. We chose this one—a high-quality, no additive option free from major allergens—that was recommended by many mamas in an eczema support group.
- Histamine intolerance is something to be aware of and to consider researching. If it wasn’t for my food journaling, I don’t think I would have ever uncovered Histamine Intolerance (HIT). I couldn’t figure out why low-allergen foods I consumed were still causing Nugget regular flare ups that presented when she nursed. It just didn’t make sense.
Until I did some googling and came across a holistic nutrition blogger’s post about HIT. (I so wish I remembered the source so I could give her credit!) . While medical resources can describe HIT in detail, I think of this condition as the cup that runneth over. If you consume too many foods known to be high histamine, your body essentially has histamine overload and can’t offload histamines as quickly as you’re introducing them. HIT can materialize in various ways. For people with AE, skin flare ups is one of these ways. Ah ha!
I was making up for nutrient deficiencies from foods I couldn’t eat by regularly eating nutrient-dense foods such as salsa, spinach, avocados, beans, bananas, grapes, strawberries, and beer and brewers yeast (to help with my dwindling milk production). All of these foods are high in histamines, or histamine releasers.
I decided to meet with a dietician to start balancing my diet with lower histamine foods, and I immediately noticed a significant difference. It was as though we were able to give her gut the time and opportunity it needed to heal. Now, she can eat plenty of high histamine foods with minimal red cheeks, if any. Certainly no reactions near what she used to have at her worst. - Creams, ointments and lotions are not created equal. We learned that ointments are better than creams, but creams are absolutely better than lotions. Avoid lotions because they have extra alcohol-based thinning ingredients that can dry out your baby’s skin. Opt for ointments or creams which are thicker and, although more annoying to handle because they can quickly stain clothes, better for eczema babies.
How can I manage my baby’s eczema?
There are many different skin care regimens your doctor might prescribe. At a minimum, these will include bleach baths, hydration regimens after bath and routine skin care to heal, repair and protect sensitive baby skin. Here are my top 9 secrets for managing baby eczema, but consider starting with the following skin care maintenance:
- Bleach baths can help manage the risk of infection that comes with broken, weepy skin. Before it reaches a point of staph infection and antibiotics are required, bleach baths (with the amount of bleach equivalent to chlorine in a pool) can help kill harmful bacteria. Use lukewarm water to avoid excessive irritation. You can learn about how to do a bleach bath and why it’s beneficial here.
- After a bleach bath, or any bath, it is very important to rehydrate your baby’s skin with a hydration regimen. Allergist-recommended, skin-healing products such as CeraVe Moisturizing Cream, Vanicream, or Eucerin Baby Eczema Cream work well for eczema babies. Aquaphor is commonly recommended but it did not work for us. Also, if your baby has a soy allergy, avoid this product because the glycerin in Aquaphor is derived from soy. (Helpful hint: Many of these products can be pricey when buying them on a regular basis. Ask your doctor or allergist to write a prescription for otherwise over the counter products to submit to health insurance alongside your receipt for reimbursement.)
- For best results, within three minutes of removing your baby from the bath, apply moisturizing cream or ointment. Instead of rubbing off excess water, use it to your advantage to help hydrate. You may wish to apply hydrocortisone or the prescribed steroid first to affected areas, then lather with your cream of choice. Apply Vaseline over top of the cream to lock in the moisture.
- Consider wet wrapping when your baby’s skin is really dry. As part of your hydration regimen, soak cotton clothing meant for wet wrapping such as this (or we use this gauze) in lukewarm water. Wrap the gauze or garment around your baby’s skin. Layer a dry cotton garment over top of the wet clothing or gauze and leave it on for a couple of hours or overnight. We did this several times on Nugget’s head (using a hat) and on her ankles when the cracks used to split open. By morning her skin was so soft and clear.
- Adopt a habitual skincare routine. Diligent skincare is the secret sauce to managing baby eczema. Trial and error will help you determine what works for your baby. Some babies only need their hydration regimen (or some form of it) done once a day before bed. While others will require frequent reapplications throughout the day (such as before naps or during diaper changes), or after they’ve been exposed to triggering environmental allergens. Remaining proactive will keep flare-ups to a minimum and ensure your baby has the healthiest skin possible.
All of this information was critical insight that informed decisions along Nugget’s eczema journey. Maybe it was our diligence to maintain the suggestions I cover here, but overall, once we had the collective information I’ve shared, managing her flare ups turned a corner and became much easier. I hope you’ve learned something from our experience to help you on your journey. <3
Eczema is a very stressful journey no mama should have to go through alone. If you are interested in joining the Facebook support group I belong to, please let me know and I will add you. Know another mama who is struggling? Please pin or share this post. Don’t forget to subscribe and let the good stuff come to you!
Other articles that might interest you
Cow’s Milk Allergy in Children – World Allergy Organization
Eczema, AD & Allergies: What is the Connection?




Hi Kim, this is so interesting and I think you are 1000% correct in when skin barrier is damaged they can become intolerance or callergic to things that might not have affected them before. May I ask what you did about the cat? We have a golden retriever and I’m wondering if the same thing has happened with us. Just wondering how you managed.. did you re home?
Hi Lyn, surprisingly our allergist didn’t recommend it. He said cat dander specifically can take years to remove and he understands animals can be part of the family. But we did everything we could to limit the contact. I vacuumed the floors daily, had an air purifier in the bedroom and playroom and kept the doors closed. It was difficult (especially during the crawling stage) but ironically we just had her tested again and the cat was the only thing she didn’t still react to! She will literally hug the cat now 🤦🏼♀️ The doctor mentioned something called Thanksgiving syndrome where kids can develop a tolerance to their own animals but the pediatrician also warned it can go the opposite way and prolonged exposure can cause asthma. It’s so tough! Good luck with your little one. ♥️